Perimenopause, the transitional phase before menopause, brings numerous physical changes that can affect skin health in unexpected ways. For many women, this hormonal shift coincides with the onset or worsening of rosacea, a chronic skin condition that is characterized by facial redness, visible blood vessels, and sometimes bumps or pustules.
Understanding the relationship between these two conditions can help you better manage your skin health during this significant life transition. Let’s explore the connection between perimenopause and rosacea and discover effective strategies to keep your skin calm and healthy during hormonal fluctuations.
What Is Perimenopause?

Perimenopause typically begins in a woman’s 40s but can start as early as the mid-30s. During this phase, the body gradually produces less estrogen, leading to irregular menstrual cycles and various other symptoms that can affect multiple systems in the body, including the skin.
The hormonal fluctuations during perimenopause can last anywhere from 2 to 8 years before menopause officially begins. These hormonal changes don’t just affect reproductive health, they can significantly impact your skin’s behavior and appearance.
How Does Rosacea Present During Perimenopause?
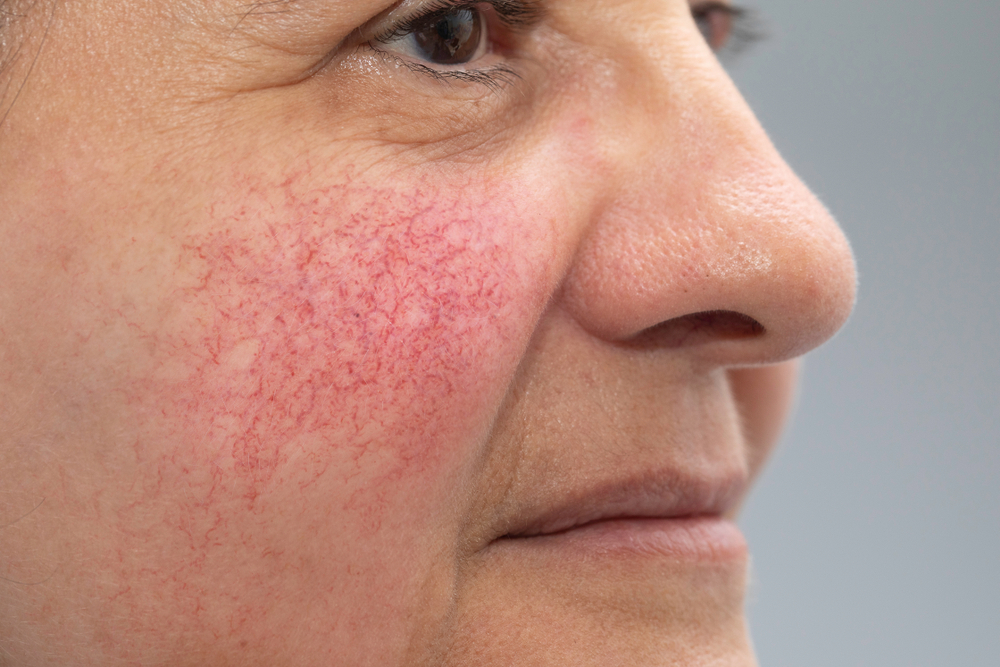
Many women notice either the first appearance of rosacea or a worsening of existing symptoms during perimenopause. The condition often manifests as persistent redness across the cheeks, nose, chin, or forehead and a tendency to flush or blush easily.
Some women also experience small, red, pus-filled bumps that may resemble acne, as well as visible blood vessels and a burning or stinging sensation on the affected skin. In more severe cases, the skin may become thicker, especially around the nose, and the eyes may become irritated or bloodshot.
Why Does Perimenopause Trigger Rosacea?
The connection between perimenopause and rosacea mainly centers around hormonal changes. Estrogen, which generally has an anti-inflammatory effect on the skin, decreases during perimenopause. This can potentially leave skin more vulnerable to inflammation.
Also, these hormonal fluctuations can affect blood vessel function, making them more reactive and leading to increased flushing and persistent redness. The skin’s natural barrier function may also become compromised during this time, making it more sensitive to environmental triggers and irritants.
Dr. Amber Kyle, board-certified dermatologist at Golden State Dermatology in Torrance, CA, explains:
“The relationship between hormones and skin inflammation is complex but significant. During perimenopause, declining estrogen levels can trigger inflammatory responses in the skin, exacerbating conditions like rosacea. We often see patients experiencing their first significant rosacea flare-ups during this transitional period, even if they’ve never had skin sensitivity issues before. Understanding this connection allows us to develop treatment strategies that address both the hormonal aspects and the skin manifestations simultaneously.”
Can Hot Flashes Worsen Rosacea Symptoms?
Hot flashes, one of the most common symptoms of perimenopause, can definitely trigger or worsen rosacea flare-ups. These sudden feelings of warmth can cause facial blood vessels to dilate rapidly, leading to intense flushing and redness.
The internal temperature fluctuations that occur during hot flashes can be particularly challenging for women who also have rosacea. Managing both conditions often requires a comprehensive approach addressing both hormonal changes and skin sensitivity.
What Skincare Adjustments Should You Make?
During perimenopause, your skin’s needs change significantly, requiring adjustments to your skincare routine. Gentle, non-irritating products become even more crucial for those experiencing rosacea flare-ups.
Look for skincare products specifically formulated for sensitive, redness-prone skin. Avoid ingredients like alcohol, fragrance, and harsh exfoliants that can trigger inflammation. Your dermatologist at The Menkes Clinic can recommend appropriate cleansers, moisturizers, and sunscreens that calm rather than aggravate your skin during this transitional period.
There are also several advanced treatment options that can effectively manage rosacea during perimenopause. Prescription topical medications like metronidazole, azelaic acid, or ivermectin can help reduce inflammation and redness.
For more severe cases, oral medications such as antibiotics or isotretinoin may be recommended. Laser and light therapies can also effectively target visible blood vessels and reduce persistent redness for long-lasting relief.
Kim Rufkahr, RN at Golden State Dermatology in Mountain View, offers insight from her clinical experience:

“We’ve seen remarkable success combining traditional rosacea treatments with lifestyle modifications for our perimenopausal patients. Many women don’t immediately connect their changing hormones with their skin issues, which can lead to frustration when typical treatments don’t provide complete relief. By addressing both aspects—using appropriate topical treatments while also implementing dietary adjustments, stress management techniques, and sometimes hormonal therapy in coordination with their primary care provider—we can help patients achieve much better control over their rosacea symptoms during this challenging transition.”
What Lifestyle Changes Can Help Manage Both Conditions?
Managing rosacea during perimenopause often requires a holistic approach beyond just skincare. Staying cool by avoiding overheating during exercise, hot weather, or hot flashes can significantly reduce flare-ups.
Protecting your skin from sun exposure is especially important, as UV radiation can trigger and worsen rosacea symptoms. Using broad-spectrum, non-irritating sunscreen daily and seeking shade during peak sun hours can significantly improve symptom management.
Can Hormone Therapy Help With Rosacea?
For some women, hormone replacement therapy (HRT) prescribed for perimenopausal symptoms may have the added benefit of improving rosacea. The estrogen in HRT can help stabilize the inflammatory responses that trigger rosacea flare-ups.
However, hormone therapy isn’t right for everyone, and the decision to use HRT should be made in consultation with both your dermatologist and gynecologist, considering your complete medical history and risk factors. Other hormonal treatments specifically targeting the skin may be more appropriate in some cases.
When it’s Time to See Your Dermatologist
If you’re experiencing persistent facial redness, flushing, or bumps that coincide with perimenopausal symptoms, it’s time to consult a dermatologist. Early intervention can prevent rosacea from worsening and help you establish an effective management plan.
A board-certified dermatologist can distinguish rosacea from other skin conditions that may look similar and develop a treatment plan tailored to your specific needs during this hormonal transition. They can also help you identify your personal triggers and develop strategies to avoid them.
If you’re experiencing perimenopausal symptoms along with skin changes like redness, flushing, or bumps, don’t wait to seek professional help. If you have questions about your skin, schedule an appointment at The Menkes Clinic today!